Introduction
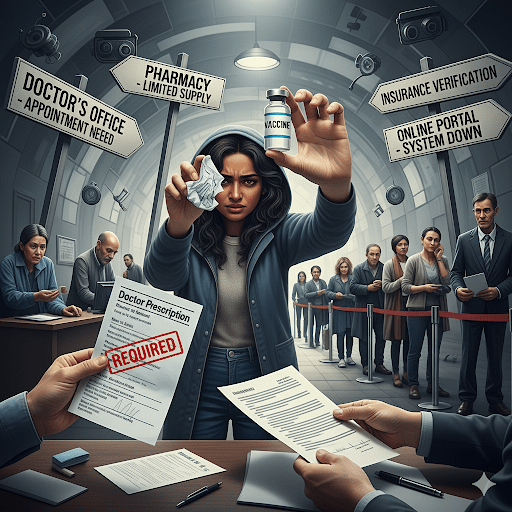
My wife’s recent attempt to schedule a COVID-19 vaccination in New York City brought into sharp focus a profound shift in U.S. public health policy. What was once a straightforward, widely accessible process had become a confusing and difficult administrative hurdle. She discovered that our local pharmacies, which previously served as convenient hubs for vaccination, no longer had a supply of doses and were requiring a doctor’s prescription for many people. This frustrating experience reveals the direct, real-world consequences of a new approach to public health that has replaced universal access with a targeted, risk-based strategy. This paper will detail the differences between the current and previous administrations’ handling of COVID-19, explore the political irony of these changes, and examine the disproportionate burden placed on low-income and rural citizens, concluding with an analysis of the potential dangers to the nation’s health.
A Shift from Universal to Targeted Access

Previous Policy Current Policy
The previous administration’s handling of COVID-19 was largely defined by a strategy of universal access. The goal was to make vaccines as widely available as possible, with the Centers for Disease Control and Prevention (CDC) recommending them for nearly everyone over the age of six months. The Food and Drug Administration (FDA) issued Emergency Use Authorizations (EUAs) that facilitated rapid distribution, enabling pharmacies, hospitals, and pop-up clinics to provide shots without a prescription.
In stark contrast, the current administration has ended these broad EUAs. The new policy restricts the FDA’s formal approval of updated vaccines to two specific groups: individuals aged 65 and older, and those between six months and 64 years old with a high-risk underlying health condition. This has created a logistical “patchwork” where states must navigate new regulations without clear, consistent federal guidance. In states like New York, the lack of a universal CDC recommendation means that pharmacists, who previously served as the primary vaccinators for nearly 90% of the population, are now legally restricted and require a doctor’s prescription for many adults.
The Irony of “Depoliticizing” Public Health
The administration has framed its new approach as an effort to “depoliticize” the issue and restore “common sense” to public health. However, the actions taken have had the opposite effect, creating a new, highly political conflict. The most potent evidence for this irony includes:
- Dismantling the CDC’s Advisory Panel: The administration’s Health and Human Services (HHS) Secretary, a well-known vaccine skeptic, fired the entire Advisory Committee on Immunization Practices (ACIP) and replaced it with a hand-picked panel. This action undermined the committee’s long-standing role as an independent, science-based body and has been seen by public health experts as a move to inject political ideology into a critical scientific process. The new ACIP panel is scheduled to meet on September 18th and 19th to discuss and vote on new recommendations for COVID-19 vaccines and other routine immunizations. The outcome of this meeting is highly anticipated and is expected to set a new direction for vaccine policy.
- Contradictory Guidance: The administration’s pronouncements often contradict the recommendations of leading medical societies like the American College of Obstetricians and Gynecologists (ACOG) and the American Academy of Pediatrics (AAP). This conflicting information creates confusion for the public, leading to decreased trust and a reluctance to follow any guidance. A key example of this contradiction is the administration’s pronouncement that COVID-19 vaccines are no longer recommended for “healthy” pregnant women and children. ACOG immediately and strongly reaffirmed its recommendation that all pregnant, recently pregnant, or lactating individuals get vaccinated, citing the increased risk of severe illness and death from COVID-19 in this population. Similarly, the AAP, in a significant break from three decades of aligning with the CDC, issued its own recommendations that all children ages six to 23 months receive the vaccine and that it should be available to any child whose parents wish to have them vaccinated.
- Creating a Fragmented System: By ending the federal government’s centralized, universal response, the administration has forced states to fend for themselves. This has led to a highly fragmented system where a person’s access to a vaccine can depend on their state of residence and the specific policies of their local pharmacy chain. This is not depoliticization; it is the implementation of a new, politically motivated system that lacks cohesion and clarity.
A Disproportionate Burden on Low-Income and Rural Citizens
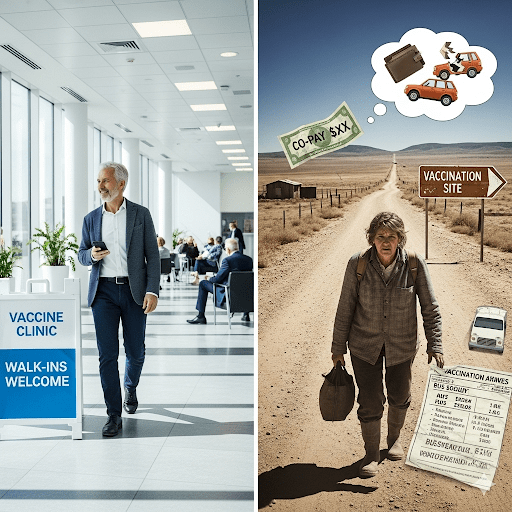
The shift to a targeted, doctor-centric model disproportionately harms low-income and rural communities, including many of the administration’s own supporters. This is not a matter of political alignment but of socio-economic reality.
- Barriers to Access: Low-income individuals face significant hurdles in getting a doctor’s prescription. They may lack the financial means for co-pays or face the impossible choice between taking an unpaid day off from work and getting vaccinated. In rural areas, these problems are compounded by a lack of healthcare providers and limited public transportation, making a simple doctor’s visit a major logistical and financial challenge.
- The Loss of Safety Nets: Other recent policies, including significant cuts to Medicaid and the expiration of Affordable Care Act (ACA) subsidies, further exacerbate these health inequities. A study from UC Berkeley estimates that these cuts and non-renewals will lead to a rise in the number of uninsured Americans, placing an even greater burden on already struggling individuals and the safety-net hospitals and clinics that serve them.
Economic status has long been a powerful predictor of health outcomes, with lower-income populations systematically experiencing worse health. The new administration’s policies, by adding bureaucratic hurdles and financial burdens to the healthcare system, are likely to worsen this trend, making it harder for low-income citizens to receive life-saving care.
Rebuttal: The Reality of Barriers for Low-Income Citizens
A detractor might argue that taking time off work has always been a barrier for low-income citizens, regardless of who is in power, and that the new rules do not make the situation more difficult. While it is true that taking time off work has always been a challenge, this argument fails to account for the new and compounded barriers that the current policy has created. The previous administration’s guidelines, while not perfect, actively worked to mitigate these issues.
First and most importantly, the prior policy of universal access eliminated the need for a doctor’s visit to obtain a vaccine. Vaccinations were widely available on a walk-in basis or through a quick, easy appointment at a local pharmacy. For many, a pharmacy is more conveniently located and has more flexible hours than a doctor’s office. The new rule, by requiring a separate trip and appointment with a physician for a prescription, adds a minimum of one extra logistical and financial hurdle.
Second, the new policy introduces a fresh layer of financial risk. The cost of a co-pay for a doctor’s visit, which was not required for a simple pharmacy vaccination, is a new barrier. Additionally, the uncertainty of insurance coverage for “off-label” prescriptions for healthy individuals creates the potential for out-of-pocket costs of over $150. Under the previous guidelines, the vaccine was federally funded and guaranteed to be free, thus removing a key financial barrier.
The new policies do not simply maintain an existing difficulty; they actively create new, specific burdens that are most acutely felt by those with the fewest resources. It is not just about taking time off work; it is about the new, mandatory steps and costs that have been inserted into the process, making it demonstrably more difficult for low-income citizens to access a critical public health service.
The Documented Impact of the COVID-19 Pandemic
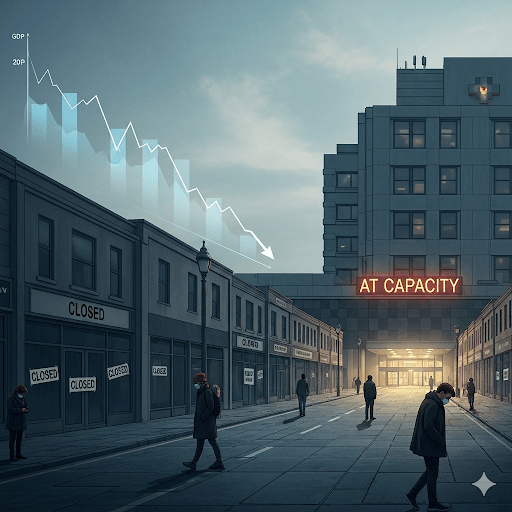
Some may argue that the threat of COVID-19 was overblown and the response was an unnecessary politicization of a minor health issue. However, the data on the damage caused by the pandemic is staggering and irrefutable, demonstrating the very real and devastating consequences of the virus.
- New York City: As the initial epicenter of the pandemic in the United States, New York City was hit particularly hard. By April 2023, the city had recorded over 2.7 million confirmed cases and more than 45,000 confirmed deaths, with thousands more probable deaths. In the early months, the city’s infection rate was five times higher than the rest of the country, and it accounted for nearly a quarter of all U.S. deaths. The economic toll was also severe, with a record 23% drop in private-sector employment and a skyrocketing unemployment rate that peaked at over 20%.
- United States: On a national scale, the pandemic’s impact was equally catastrophic. The U.S. has recorded over 1.1 million deaths from COVID-19. The economic consequences were unprecedented, with real GDP contracting by 3.5% in 2020—the first decline since the Great Recession. The unemployment rate surged to 14.7%, and millions of workers were dislocated from their jobs.
- Globally: The pandemic’s reach was global and its effects were felt in every corner of the world. The World Health Organization (WHO) has reported nearly 7 million deaths, though the actual number is believed to be much higher due to underreporting. The global economy was devastated, with a projected loss of over $8.5 trillion in output over two years, wiping out nearly all gains from the previous four years. In low- and middle-income countries, the pandemic led to a dramatic rise in inequality, and for the first time in a generation, global poverty increased.
Beyond the immediate loss of life and economic devastation, the long-term health consequences of COVID-19, known as “long COVID,” continue to affect millions of people. This condition can lead to persistent and debilitating symptoms, including extreme fatigue, “brain fog,” and organ damage, further straining both the healthcare system and the economy. The data clearly shows that COVID-19 was not a minor health issue; it was a global catastrophe with profound and lasting health, social, and economic consequences.
Conclusion: The Dangers of the New Approach
The current administration’s handling of COVID-19 vaccinations, while framed as a move toward personal freedom and reduced government overreach, carries significant potential dangers for the health and well-being of the nation. The policy changes, which have led to confusion and restricted access, are likely to result in:
- Lower Vaccination Rates and Increased Disease Spread: The barriers created for the general population could lead to a decline in vaccination rates, increasing the risk of larger and more severe outbreaks, particularly in vulnerable communities.
- Erosion of Public Trust: The political interference in public health agencies and the issuance of conflicting guidance undermine public confidence in science and government institutions. This erosion of trust could make it harder to respond effectively to future health crises.
- Exacerbation of Health Disparities: By creating new administrative and financial hurdles, the new policies disproportionately harm low-income and rural populations, exacerbating existing health inequities and placing a greater burden on the most vulnerable members of society.
- Further Uncertainty from the ACIP Meeting: The upcoming ACIP meeting, with its new, politically-appointed members, has the potential to add to this chaos. If the committee issues recommendations that further narrow eligibility or conflict with the guidance of other medical societies, it could deepen the confusion, lead to further drops in vaccination rates, and raise new questions about insurance coverage and liability.
This case study of a simple attempt to get a vaccine in New York reveals a much larger problem: a public health policy that, by prioritizing political ideology over proven public health principles, may be inadvertently jeopardizing the health of the very people it claims to protect.
Edward Odom

